Review Article
Incisions And Prevention of Stigmata Related to Deep Plane Rhytidectomy: A Systematic Scoping Review
- Jorge Alberto Espinosa Reyes MD
Corresponding author: Jorge Alberto Espinosa-Reyes, MD, ENT, Facial Plastic Surgeon Calle 127a # 7- 53 cons 3005 (INO), Bogotá, Colombia, ORCID: 0009-0008-7673-586x
Volume: 1
Issue: 1
Article Information
Article Type : Review Article
Citation : Jorge Alberto Espinosa Reyes MD, Juan Fernando Muñoz MD, Roxana Cobo MD, Nicolás Heredia MD, Gabriela Menjivar MD, Juan Gabriel Camacho Triana MD, Juan C. Ochoa MD. Incisions And Prevention of Stigmata Related to Deep Plane Rhytidectomy: A Systematic Scoping Review. Journal of Surgery Research 1(1). https://doi.org/10.61615/JSR/2025/SEPT027140930
Copyright: © 2025 Jorge Alberto Espinosa-Reyes, MD. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.61615/JSR/2025/SEPT027140930
Publication History
Received Date
02 Sep ,2025
Accepted Date
19 Sep ,2025
Published Date
30 Sep ,2025
Abstract
Rhytidectomy has evolved since 1990, when Hamra described the deep plane approach to elevate the midface soft tissue and improve the nasolabial folds. Since then, this technique has changed how facial rejuvenation is approached worldwide. The experience exposed in books and articles was evaluated through a systematic scoping review to show interventions and preventive measures described in the deep plane rhytidectomy. PROSPERO has not registered any systematic review related to stigmata in facelift. We aim to describe incisions and preventive strategies to minimize postoperative stigmata in deep-plane rhytidectomy. Therefore, the following databases: PubMed, Web of Science, Scopus, and The Cochrane Library were searched from January 1990 to January 2023.
In conclusion, this systematic scoping review synthesizes information related to the incisions, stigmata, and preventive strategies in the deep plane rhytidectomy, providing an easy categorization.
Keywords: Rhytidectomy, Facelift, Rhytidoplasty, tell-tale signs, Stigmata, Face rejuvenation.
►Incisions And Prevention of Stigmata Related to Deep Plane Rhytidectomy: A Systematic Scoping Review
Jorge Alberto Espinosa Reyes MD1*, Juan Fernando Muñoz MD2, Roxana Cobo Sefair MD3, Nicolas Heredia Combariza MD4, Gabriela Maria Menjivar Huezo MD5, Juan Gabriel Camacho Triana MD6, Juan Carlos Ochoa Álvarez MD7
1ENT, Facial Plastic Surgeon, Calle 127a # 7- 53 cons 3005 (INO), Bogotá, Colombia, ORCID: 0009-0008-7673-586x
2ENT, Facial Plastic Surgery fellowship – The Face & Nose Institute. Bogotá, Colombia, ORCID: 0000-0002-0158-1623
3ENT, Facial Plastic Surgeon, Cali, Colombia, ORCID: 0000-0002-3658-6256
4ENT, Professor in Facial Plastic Surgery Fellowship, Bogotá, Colombia, ORCID: 0000-0002-7691-1746
5ENT, Facial Plastic Surgery fellowship – The Face & Nose Institute. Bogotá, Colombia, ORCID: 0009-0004-7764-6050
6ENT, Facial Plastic Surgery fellowship – The Face & Nose Institute. Bogotá, Colombia, ORCID: 0000-0001-9974-4162
7ENT, Facial Plastic Surgery fellowship – The Face & Nose Institute. Bogotá, Colombia. ORCID: 0009-0003-5224-0663
Introduction
When patients consult for aesthetic plastic surgery, they usually look for natural-appearing outcomes, which is why one of the questions during their first visit is about scars. Each detail about incision planning must be considered when a rhytidectomy is being planned, and the experience of each facial plastic surgeon has excellent value, making a difference in the long-term satisfaction and fulfillment of patient expectations.
Rhytidectomy has evolved since 1990, when Hamra described the deep plane approach to elevate the midface soft tissue and improve the nasolabial folds1. Since then, this technique has changed the way we approach facial rejuvenation around the world. It is well known that with the deep-plane approach, there is a significant amount of flap mobilization, and additionally, the tension is not transferred to the skin. We aim to describe incisions and preventive strategies to minimize postoperative stigmata in deep-plane rhytidectomy. This will be achieved by conducting a scoping review of reports from 1990 to 2023. Given the lack of controlled trials on this topic, the review will include books and articles.
Methods
Protocol and Registration
This study was designed as a systematic scoping review due to the necessity to evaluate different medical literature sources and the limited number of clinical trials on the topic. A protocol was used, but not formally registered. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) guideline was considered2. This review could not be registered in PROSPERO because they do not accept scoping reviews.
Eligibility Criteria
The review included articles and book chapters discussing incisions and preventive strategies to avoid stigmata during deep-plane rhytidectomy. Gray literature was not included, and only publications written in English were considered.
Information Sources
From January 1990 to January 2023, the following bibliographic databases were searched: PubMed, Web of Science, Scopus, and The Cochrane Library. The search strategy was designed by an author with formal education in systematic reviews.
Search
The electronic search strategy included the keywords Facelift, Face-lift, Rhytidectomy, rhytidoplasty, and deep plane as follows:
((((face lift[Title/Abstract]) OR (facelift [Title/Abstract])) OR (rhytidectomy[Title/Abstract])) OR (rhytidoplasty[Title/Abstract])) AND (deep plane)
Selection of Sources of Evidence
All reviewers screened the same number of publications and discussed the results. Two reviewers with the most experience in deep-plane rhytidectomy worked in pairs and evaluated the full-text publications. When disagreement on study selection was presented, it was resolved by consensus.
Data Charting Process and Data Items
Two reviewers jointly developed a data-charting form to determine which qualitative variables to extract. The two reviewers worked independently and discussed the results.
Data on: incisions description according to superficial anatomy at the temple-temporal, preauricular, lobule, postauricular, and mastoid-occipital areas, besides the author's preventive strategies and stigmas prevented.
Synthesis of Results
We organized the incision information, categorizing them by five skin areas (temple/temporal, preauricular, lobule, postauricular, and mastoid-occipital) and summarizing them with a figure. Based on the authors ' opinions in each report, one table presents the relationship between preventive strategies and stigmata prevented.
Results
A total of 1164 records were retrieved from database searches. After removing duplicates, 1147 abstracts were screened for eligibility. Thirty-three records were excluded because they were related to cadaveric descriptions, animal studies, neck lifts without facelifts, or procedures without an aesthetic purpose. Subsequently, 1133 reports were assessed in full text. Of these, 1109 reports were excluded because incisions were not described or deep plane rhytidectomy was not mentioned. Other sources included two additional articles to confirm the authors' incisional approach. Finally, 26 reports, including original articles and book chapters, were included [3-29]. No clinical trials were found.
Characteristics of Incision Design
Information about incisions performed during deep plane rhytidectomy. Figure 1.
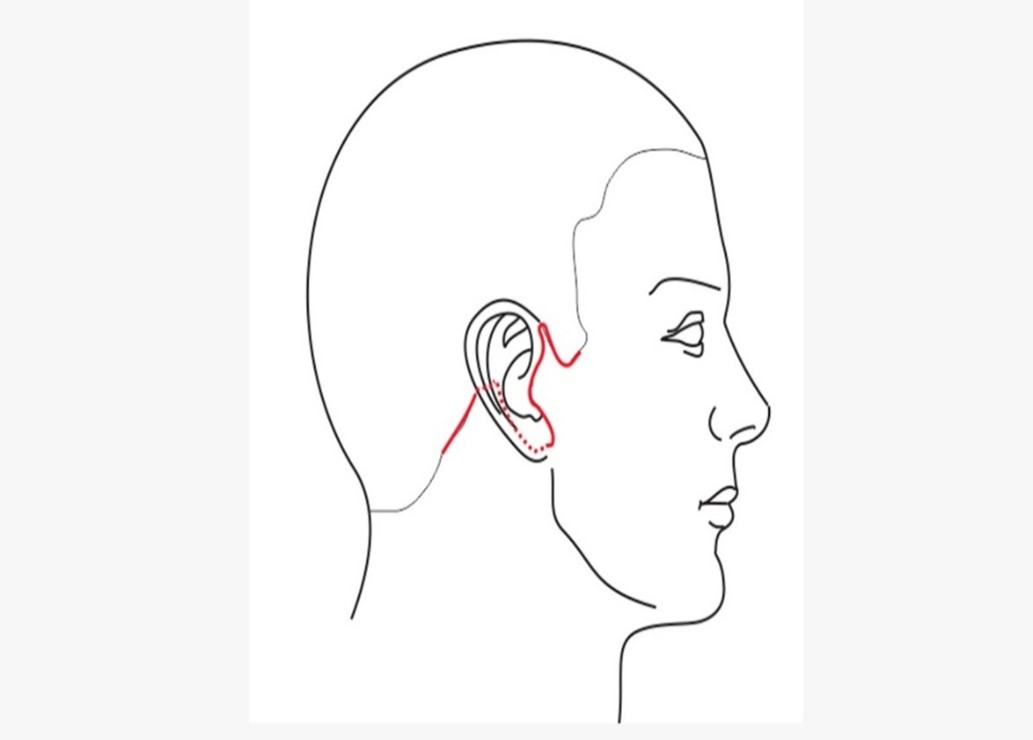
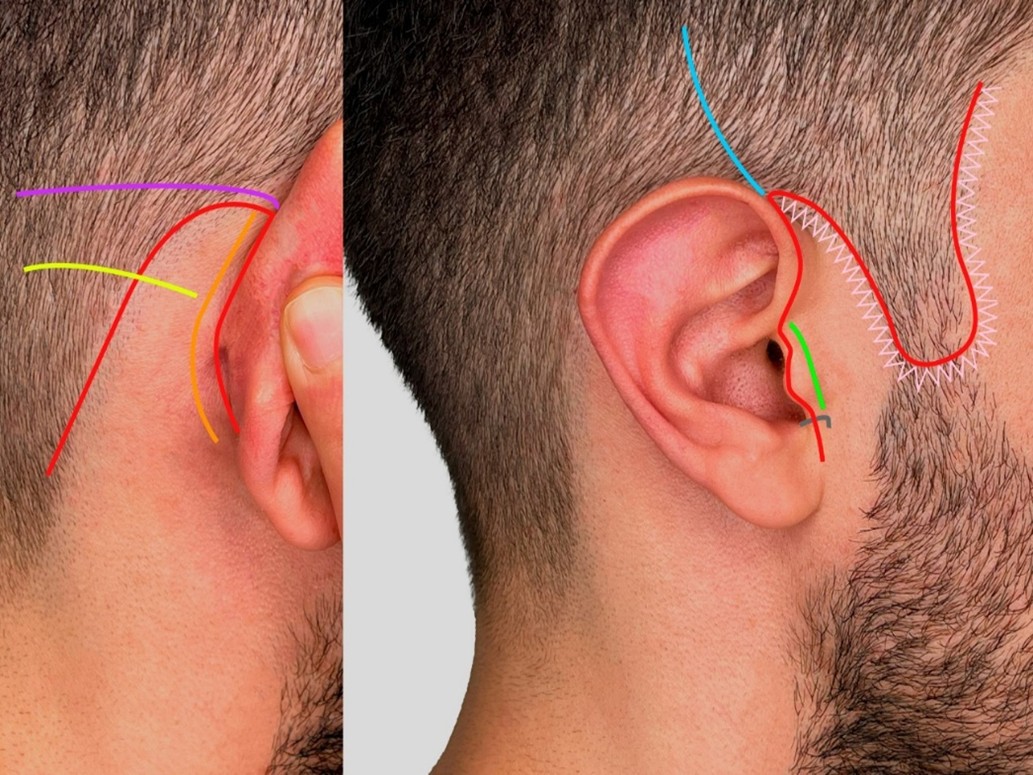
Figure 1. Deep Plane Rhytidectomy Incisions
Results of Stigmata and Prevention Strategies
For each original article or book chapter, stigmata information was extracted, along with strategies recommended by the authors to prevent their development. Table 1.
Table 1. Techniques Advocated to Reduce the Risk of Stigmata of Deep Plane Facelift
|
Stigma Prevented |
Techniques Advocated to Reduce the Risk of Stigma |
Bibliographic Reference |
|
Dog ear deformity or extra wrinkles |
|
1,17, 20, 26 |
|
Temporal alopecia Temporal visible scar Temple visible scar Step off sideburn
|
|
3,4,24
7,12,20
3,4,9,23,24
3,11,19,21,23 |
|
Unnatural shifts of the hair. Root of the helix with a wide appearance Blunt tragus Outwardly protruding tragus Unnatural skin contouring of the tragus or loss pretragal crease Transplanting hair-bearing skin onto the tragus the pinching of the incisura antitragus hair-bearing skin into the external auditory canal
|
|
22
7,12,20
7,10,12,20
27
22,24
8,13,14,19
7,12, 13, 20, 22
23 |
|
Pixie ear deformity
|
|
7, 11,12,20,26 |
|
Posterior auricular visible scar |
|
7,12,16,20
|
|
Disturbance of the natural mastoid hairline Mastoid visible scar Step-off occipital-mastoid hairline
|
|
11,2 23
16,17
24,27 |
Synthesis of Results
Information divided by zones Temple/Temporal (T), Preauricular (P), Lobule (L), Postauricular (PA), Mastoid-Occipital (MO) showed:
T: A temporal hairline incision [7,8,10-12,16,18-20,25,26] vs. in the temporal tuft and extension just superior to the helical root [3-6,9,11,13,14,21,22,23,24] including bald men17. The first incision was recommended because an excess skin flap was generated, and the second one was considered for cases where temporal lifting is desired. A low-lying sideburn was considered [3,4,21,24].
P: Incision should follow the natural highlight, keeping the width of helical crus intact [7,12,15,18,20,25]; afterward, it may be retrotragal in women and pretragal in men [3-12, 14-28]. An inferior step under the anterior tragus could be designed [7,12,15,18,20,25]
L: A peri-lobular incision. A distance of 2 mm inferior to the lobule cheek junction is recommended. [7,12,13,15,18,25].
PA: Incision continues over the posterior concha, a few millimeters from the retroauricular sulcus 3-8,10-28 even. Some recommend continuing into the sulcus [9,21]. With transition placed with an acute or obtuse angle to the mastoid area (10, 19, 28) at the superior portion of the concha, external auditory canal14 or triangular fossa [7,12,13,15,18,25].
MO: Incision into the hair of the scalp with curve transition [3-5,13,21,22,26] or following the occipital hairline inferiorly [7,12,15,18,20,25], depending on the amount of flap advanced posteriorly. Some advocate for a W-plasty incision [16].
Incision descriptions, preventive strategies, and stigmata that could be prevented through categorization into four groups were considered, as shown in Figure 2.
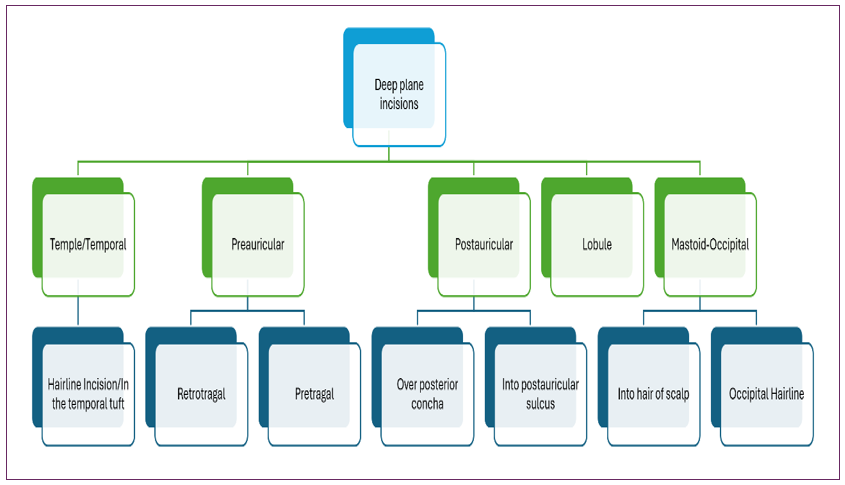
Figure 2. Categorization Proposal Stigmata Based on the Scoping Review.
In the first group, Visible scar, Temporal alopecia, Temporal visible scar, Temple visible scar, Mastoid visible scar, and posterior auricular visible scar. The second group, Skin or Hair with unnatural appearance: Dog ear deformity or extra wrinkles, Step sideburn, Unnatural shifts of the hair, Root of the helix with wide appearance, Disturbance of the natural mastoid hairline, Step-off occipital-mastoid hairline. The third group is the distortion of the earlobe: pixie ear deformity. And the fourth group, Distortion of or around the tragus: Blunt tragus, outwardly protruding tragus, Unnatural skin contouring of the tragus or loss of pretragal crease, transplanting hair-bearing skin onto the tragus, the pinching of the incisura antitragus, hair-bearing skin into the external auditory canal. Figure 3A and 3B.
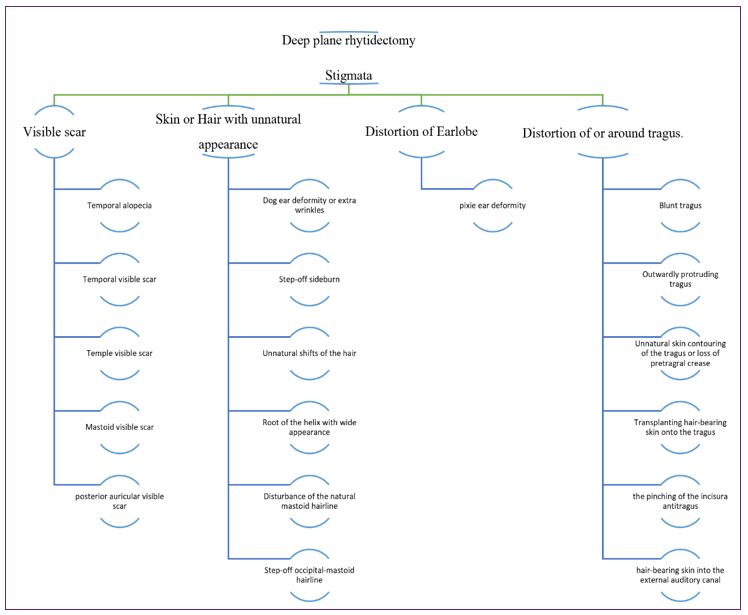
Figure 3: Categorization proposal of stigmata based on the scoping review

Figure 4A: Face Stigmata Posterior to Rhytidectomy on the Right Side

Figure 4B: Face Stigmata Posterior to Rhytidectomy on the Left Side

Natural Outcomes Without Visible Scar Malposition

Representative Case Illustrating a Favorable Outcome
Discussion
In this systematic scoping review, we considered 26 articles and book chapters [3-28], examining various incisions and stigmata, or "tell-tale signs." These were subsequently illustrated and categorized. Each report detailed the authors' approaches to preventing facelift stigmata and provided preventive strategies.
Patients seeking facial rejuvenation surgery are often unaware of stigmata. Therefore, it is crucial for the surgeon to be knowledgeable about their prevention and treatment. The surgeon must also clearly communicate the risks associated with different types of incisions. Proper patient selection for deep-plane rhytidectomy is essential, and the subsequent step is identifying the most suitable incision for each patient.
Traditional deep plane approach through long incisions has evolved for some patients who could benefit from short access with a vertical lift, like the MADE vertical face-lift described by Jacono, which does not require a postauricular occipital scalp limb[16]. Another description, by Mani, involves an endoscopic approach avoiding the preauricular scar by a tunnel that connects the temporal incision with the lower preauricular area subcutaneously, with the subsequent excess of skin that could be minimized with a more vertical vector of fixation [27]. This is a probe of how an excellent aesthetic result can be achieved with a shorter incision and a changing facelift vector. However, not all patients are candidates for these approaches.
All facelift procedures will have some scar that could be more or less important depending on the patient’s perspective. Therefore, even the less visible scar could benefit from how the surrounding tissue gives camouflage. All creases through preauricular and postauricular skin must be considered, as well as hair density or baldness. In one observational study, minimized incisions were described by Pascali, in bald men as next: at the temple, an incision between 2-4 cm with an angle of 120 degrees and posteriorly within occipital extension no more than 2 cm, with the posterior edge of the helix as a limit to achieve better scar camouflage [17].
On the other hand, the difference between men and women requires choosing between a pretragal visible scar or transplanting hair-bearing skin onto the tragus. The last one will need ancillary techniques like intraoperative follicular unit resection versus posterior laser therapy. According to an expert's opinion, 75% of men prefer incision camouflage with a retrotragal incision [12].
A survey studying surgeons comparing preferences according to incisions showed that for temporal incisions, 87% of doctors preferred "in the hairline," whereas 13% chose the "pre-hairline." For mastoid incisions, 20% preferred "in the hair," and 80% chose "at the hairline." No correlation was found between preauricular incision preferences and the years of medical practice [30]. Our results did not yield a quantitative effect that could provide a specific recommendation, as no comparative studies or new surveys are available on this topic.
There are limited articles related exclusively to stigmas. Describing them as “operated face signs” is an easy way to explain them, and no classification is well defined; even recommendations are performed independently of the facelift approach [31]. This scoping review achieves what we termed preventive strategies according to the evidence available from experienced surgeons.
Limitations
With all the information reviewed, no article included a comparison between incisions and the evaluation of preventive strategies. According to the evidence, this scoping review provides a valuable piece of medical literature if we consider that, for ethical purposes, clinical trials cannot be designed.
Another limitation related to language due to the restriction on the English language. Finally, the last limitation was that the articles were unavailable for authors to review.
Conclusion
This systematic scoping review synthesizes information related to the incisions, stigmata, and preventive strategies in deep plane rhytidectomy, providing an easy categorization. This promotes a change in how facial surgeons approach the procedure, aiming for better aesthetic results that could bring consensus between surgeons in the future.
Conflicts of Interest
All authors declared that there are no conflicts of interest.
- Hamra ST. (1990). The deep-plane rhytidectomy. Plast Reconstr Surg. 86: 53–61; discussion 62–63.
- Tricco AC, Lillie E, Zarin W. (2018). PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation Ann Intern Med. 169(7): 467-473.
- Perkins SW. (2000). Achieving the “natural look” in rhytidectomy. Facial Plastic Surgery. 13: 269-282.
- Perkins SW, Patel A. (2009). Extended Superficial Muscular Aponeurotic System Rhytidectomy: A Graded Approach. Facial Plast Surg Clin N Am. 17(4): 575–587.
- Alsarraf R, Johnson CM. (2000). The facelift: technical considerations. Facial Plast Surg. 16(3): 231–238.
- Alsarraf R, Johnson CM. (2003). The deep plane facelift. Facial Plast Surg. 19(1): 95-105.
- Jacono A, Bryant LM. (2018). Extended Deep Plane Facelift: Incorporating Facial Retaining Ligament Release and Composite Flap Shifts to Maximize Midface, Jawline, and Neck Rejuvenation. Clin Plast Surg. 45(4): 527-554.
- Raggio BS, Patel BC. (2023). Deep Plane Facelift. In: StatPearls [Internet]. 2023, Apr 3. Treasure Island (FL): StatPearls Publishing. 31424861.
- Pastorek N, Bustillo A. (2005). Deep plane face-lift. Facial Plast Surg Clin North Am. 13(3): 433-449.
- Gordon NA, Tower JI, Paskhover B. (2020). From the Deep-Plane Rhytidectomy to the Vertical Platysma Advancement. Facial Plast Surg Clin North Am. 28(3): 311-330.
- Sykes JM, Liang J, Kim JE. (2011). Contemporary deep plane rhytidectomy. Facial Plast Surg. 27(1): 124-132.
- Jacono AA. (2020). A Novel Volumizing Extended Deep-Plane Facelift: Using Composite Flap Shifts to Volumize the Midface and Jawline. Facial Plast Surg Clin North Am. 28(3): 331-368.
- Quatela V, Montague A, Manning JP, Antunes M. (2020). Extended Superficial Musculoaponeurotic System Flap Rhytidectomy. Facial Plast Surg Clin North Am. 28(3): 303-310.
- Kamer FM, Mingrone MD. (2005). Deep plane rhytidectomy: a personal evolution. Facial Plast Surg Clin North Am. 13(1): 115-126.
- Jacono AA, Rousso JJ. (2013). The modern minimally invasive facelift: has it replaced the traditional access approach? Facial Plast Surg Clin North Am. 21(2): 171-189.
- Starkman SJ, Mangat DS. (2020). Less Invasive Superficial Musculoaponeurotic System Approaches in Rhytidectomy: How, When, and Why. Facial Plast Surg Clin North Am. 28(3): 273-283.
- Pascali M, Botti C, Botti G. (2020). Face Lifting in Bald Male Patients: New Trends and Specific Needs. Plastic and Reconstructive Surgery. 145 (1): 60 – 69.
- Jacono, AA, Parikh, SS. (2011). The Minimal Access Deep Plane Extended Vertical Facelift. Aesthetic surgery journal. 31(8): 874-890.
- Gordon NA, Sawan TG. (2020). Deep-Plane Approach to the Vertical Platysma Advancement: Technical Modifications and Nuances over 25 Years. Facial plastic surgery. 36(4): 358-375.
- Jacono AA, Talei B. (2014). Vertical Neck Lifting. Facial plastic surgery Facial Plast Surg Clin North Am. 22(2): 285-316.
- Botti, C, Botti G. (2015). Facelift 2015. Facial plastic surgery. 31(5): 491-503.
- Calvin J, Murphy M. (2017). The deep plane facelift. Master Techniques in Facial Rejuvenation. 173-190.
- Barrett D.M, Gerecci D, Wang T. (2016). Facelift Controversies. Facial Plastic Surgery Clinics of North America. 24(3): 357-366.
- Rodriguez-Bruno K, Papel I.D. (2011). Rhytidectomy: Principles and practice emphasizing safety. Facial Plastic Surg. 27(1): 98-111.
- Jacono A.A, Malone M.H. (2017). Deep Plane Rhytidectomy Modifications Master Techniques in Facial Rejuvenation. 191-210.
- Holck D.E.E, Foster JA, Kalwerisky K. (2015). Ten tips for a reliable and predictable deep plane facial rhytidectomy. Pearls and Pitfalls in Cosmetic Oculoplastic Surgery second edition. 605-612.
- Walden J.L, Aston S.J. (2010). Rhytidectomy. Plastic Surgery Secrets Plus. 504-515.
- Gordon N, Adam S. (2014). Deep plane facelifting for facial rejuvenation. 30(4): 394-404.
- Mani M. (2023). Endoscopic, “Scarless” Composite Flap Face and Neck Lift. Facial plastic surgery.
- Matarasso, A, Elkwood, A, Rankin, M, Elkowitz, M. (2000). National Plastic Surgery Survey: Face Lift Techniques and Complications. Plastic and Reconstructive Surgery. 106(5): 1185-1195.
- Franco, T. (1985). Face-Lift Stigmas. Annals of Plastic Surgery. 15(5): 379–385.
Download Provisional PDF Here
PDF



p (1).png)



.png)




.png)
